Preventing infections, improving public health services, and testing new treatments have been critical to slowing the HIV/AIDS pandemic.
According to the World Health Organisation (WHO) 37.9 million people were living with HIV in 2018. Africa is the most affected region, accounting for almost two-thirds of new HIV infections.
UK research has taken an integrated approach to tackling HIV/AIDS epidemics in Low– and Middle-Income Countries (LMICs).
Supporting the global effort to achieve zero infections
UK research focused on prevention strategies has included:
‘Cash plus care’ (2009-2012)
This initiative, co-funded by ESRC and international funders, explored whether increasing adolescent access to social protection (e.g. social welfare grants and free schooling) could be an effective HIV prevention strategy in sub-Saharan Africa. They found that ‘cash plus care’ programmes helped to reduce transactional sex by 50%, older sexual partners by 70%, and unprotected sex by 50%. The approach has been adopted across 10 sub-Saharan Africa countries, potentially benefitting some 2 million adolescent girls.
Promoting circumcision for men (1997-2008)
This series of randomised controlled trials conducted by the London School of Hygiene and Tropical Medicine (LSHTM), showed that male circumcision reduced the risk of HIV infection by 48-60%. As a result, many at-risk countries in sub-Saharan Africa have initiated circumcision programmes.

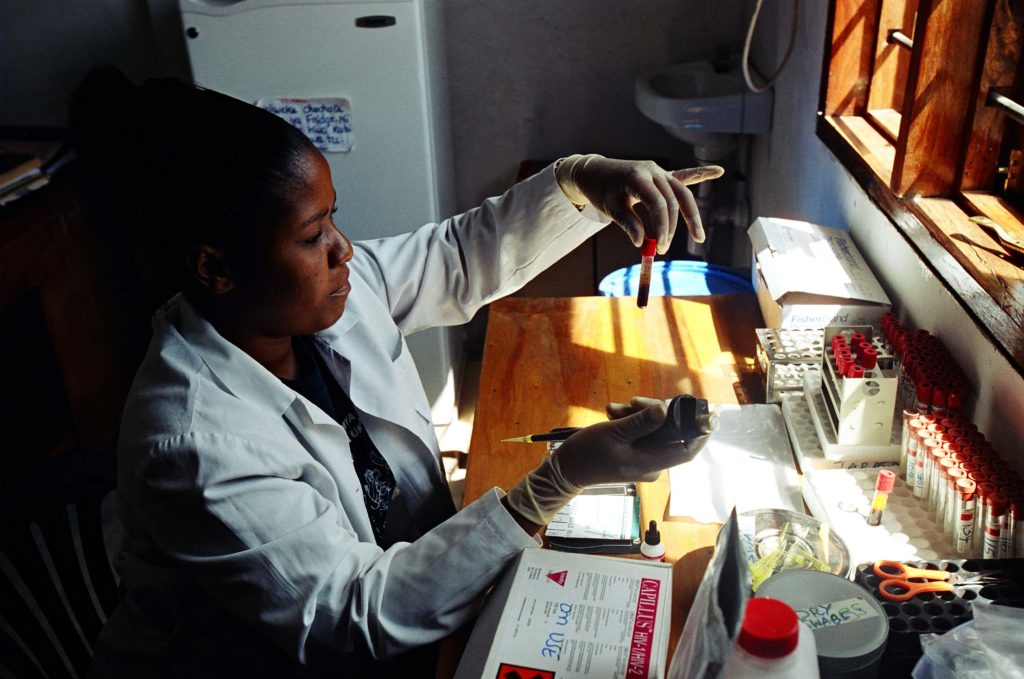
Improving the delivery of essential health services
UK research evaluating the effectiveness of healthcare provisions for people living with HIV/AIDS has informed the development of cost-effective and efficient public health systems.
Population Effectiveness of Antiretroviral Therapy to Reduce HIV Transmission (PopART) Initiative
This trial, sponsored by NIH and led by researchers at LSHTM and Imperial College London, analysed the impact of an approach, termed ‘test and treat’, on HIV incidence in South Africa and Zambia. The approach combined: universal HIV counselling and testing at household level, linking HIV-infected people with care providers, and early-stage antiretroviral therapy (ART). The study found that HIV infections were 30% lower in communities enrolled in ‘test and treat’, compared to those receiving standard care.
The Pan African Harmonisation Working Party (PAHWP)
This initiative, facilitated by LSHTM, creates a framework for harmonising regulations related to medical devices and diagnostics in Africa. It is working to ensure a new generation of diagnostic tests are used at the point of care to help prevent the spread of HIV. It is recommending ways to ensure tests are safe, effective, and accessible.
Identifying life-saving drug treatments
UK-funded (MRC, DFID, Wellcome) medical research trials have evaluated the effectiveness of antiretroviral drugs, drug combinations, and application strategies.
Development of Antiretroviral Therapy in Africa (DART) (2003-2008)
This trial (co-funded by MRC, DFID, and international funders) studied the best ways to manage ART in public health programmes in Africa and other resource-limited settings. The study showed that ART can be delivered without expensive routine blood tests – an important finding that has enhanced access to treatment.

Sustaining the charge against HIV
Between 2000–2018, new HIV infections fell by 37% and HIV-related deaths by 45%. However, there are worrying signs that prevention may be stalling. The WHO has attributed this to social and legal barriers that prevent people accessing HIV services. Research initiatives such as ‘Cash Plus Care’ and PAHWP have identified prevention strategies and supported the development of robust, responsive, and accessible public health systems. .





